Research & Articles
TMJ & SLEEP THERAPY CENTRE OF THE GORGE
TREATING CHRONIC PAIN AND BREATHING DISORDERS WITH TECHNOLOGY
Orthodontic Practice US (Volume 10 Number 2) | April 2019
Dr. Steven R. Olmos explores high-tech solutions to treatment problems
Chronic pain and breathing disorders can be effectively treated with various technologies that take the frustration out of treatment for both the clinician and the patient. Check out the variety of technologies that help Dr. Steven Olmos treat these disorders.
Educational aims and objectives:
This clinical article aims to discuss how to treat chronic pain and breathing disorders with technology.
Expected outcomes:
- Recognize how 3D imaging can be beneficial for evaluation of chronic pain and breathing disorders.
- Realize the role that low-level laser therapy can play in chronic pain treatment.
- Realize how orthodontic appliance therapy can help in treatment of chronic pain, sleep-breathing disorders, and orthopedic/orthodontic therapy.
- Identify some testing methods for these chronic pain and breathing disorder issues.
IMPROVED NASAL VOLUME UTILIZING HYPEROSMOTIC SALINE XYLITOL MIXTURE
ECronicon Open Access – EC Pulmonology and Respiratory Medicine | April 2019
by Dr. Steven R. Olmos & Dr. Joseph Baba
This paper quantifies the reduction of soft tissue hypertrophy of the nasal complex resulting in an increase of nasal volume and increased flow using a mixture of Xylitol and Saline. The health benefits of improved nasal breathing through increased inspired nasal NO (nitric oxide) and the antimicrobial benefits of Xylitol are discussed. Restoration of functional breathing (nasal) and it’s relation-ship to up righting head posture is reviewed.
Keywords: Xlear; Xylitol; Nasal Obstruction; Forward Head Posture; Nitric Oxide
ORAL APPLIANCES — PAST, PRESENT, AND FUTURE

Orthodontic Practice US (Volume 9 Number 4) | June 2018
Dr. Steven R. Olmos and Matt Rago review oral appliances and their characteristics
Oral appliances designed for relief of facial pain and jaw dysfunction, sleep breathing disorders, and orthodontics have been utilized for many years with little change in materials until recently. This article will review indications/limitations of existing designs/materials, and how computer-aided manufacturing allows for better and healthier alternatives.
There is always a reason for patients’ symptoms. Chronic face, jaw, head, and neck pain are all interrelated and are highly comorbid with sleep breathing disorders.1 Malocclusion, skeletal development deficiencies, and teeth crowding are symptoms of a functional breathing disorder.2-7 Oral appliances are used for each indication.
DIDN’T SLEEP MUCH LAST NIGHT? HERE’S HOW TO GET THROUGH THE DAY

www.nbcnews.com
These tips will help you survive the day when you’re running on empty.
Improving quality of life and faces nonsurgically
Dr. Steven R. Olmos explores how TMJ and airway issues can cause chronic health conditions
Orthodontic Practice US (Volume 8 Number 3) | March 2017
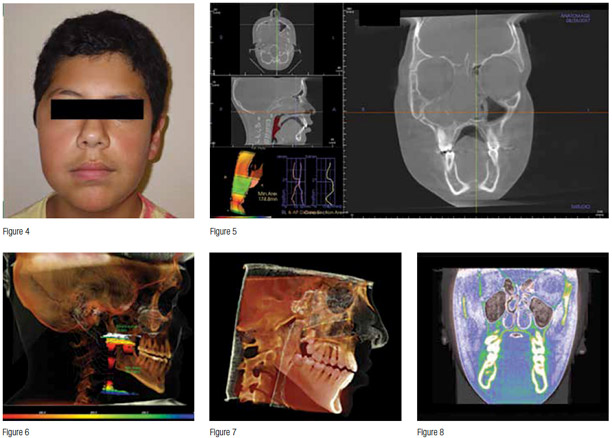
A case study featuring a young patient is presented as an example of the airwaycentered philosophy that essentially is defined as a mandibular relationship that produces the optimal orthopedic function of the temporomandibular (TM) joints and prevents or reduces airway collapse (oropharyngeal) in the unconscious state (sleep).
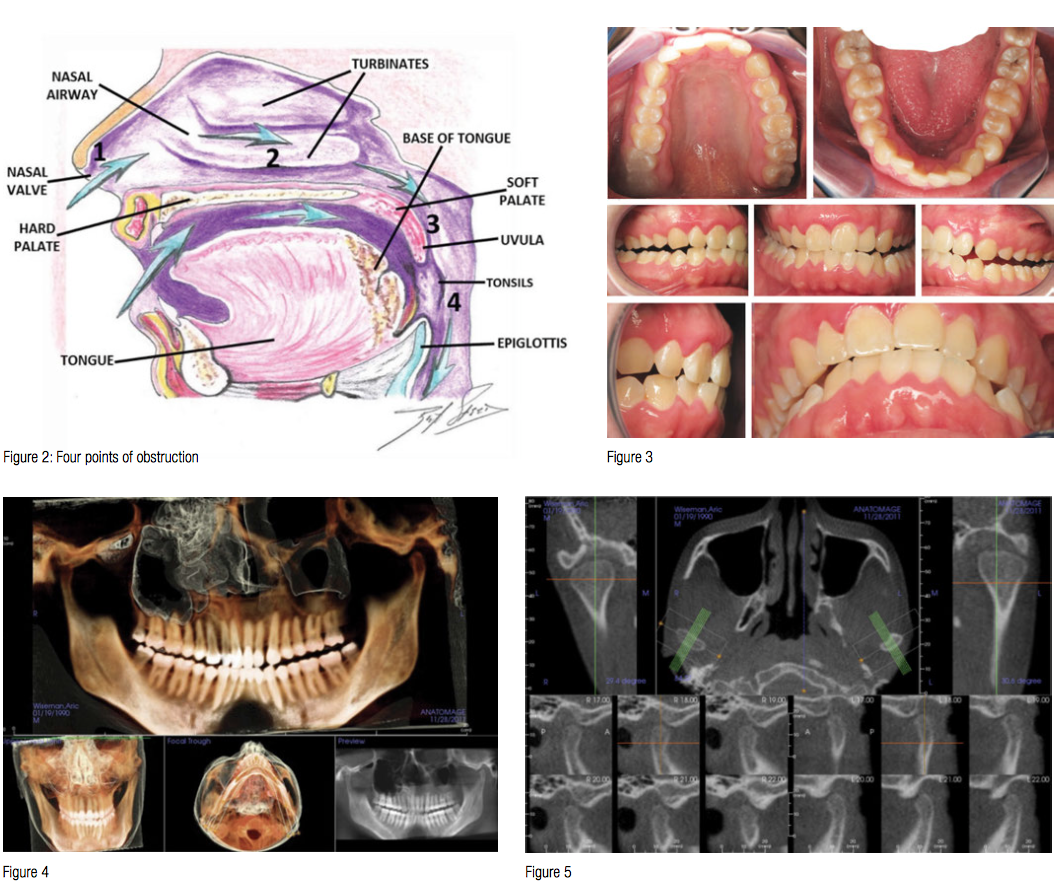
Airway Centered Dentistry: (The A, B, C’s of Treatment for Chronic Face Pain/OSA and Closing Anterior Openbite Without Ortho)
Airway Centered Dentistry: (The A, B, C’s of Treatment for Chronic Face Pain/OSA and Closing Anterior Openbite Without Ortho)
by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO
This article defines “Airway Centered Dentistry”, explains the mechanism of chronic face/jaw pain and dysfunction, reviews the technique and triage systems that have been successful in the standardized approach currently utilized in 45 TMJ and Sleep Therapy Centres in seven countries.
Chasing Pain
Diagnosing and Treating Trigeminal Neuralgia in General Dentistry
As dentists, we know quite a bit about tooth and gum pain, but when it comes to chronic facial pain and neuropathic pain, our dental school education leaves us unprepared. The objective of this article is to explain the differences between men and women with chronic orofacial pain and the relationship to proper functional breathing.
Headache and jaw locking comorbidity with daytime sleepiness

Orthodontic Practice US American Journal of Dentistry, Vol. 29, No.3 | June, 2016
Purpose: To investigate the relationship between craniofacial pain symptoms (painful conditions present in the cranium and face, including jaw joint-related pathology and primary headache conditions) and daytime sleepiness, determined by the Epworth sleepiness scales (ESS), to correlate the comorbidity as well as potential predictive factors.
Pediatric severe apnea/obesity/TMD/headache — Class III

Orthodontic Practice US (Volume 7 Number 3) | May 2016
The purpose of this case study is to demonstrate the relationship between obstructive sleep apnea (OSA), obesity, TMD, and headache in the pediatric population. It is possible to resolve OSA in children whereas we most often only manage it in the adult population. This demonstrates the need to identify the clinical signs and screen for sleep-breathing disorder symptoms in children and adolescents.
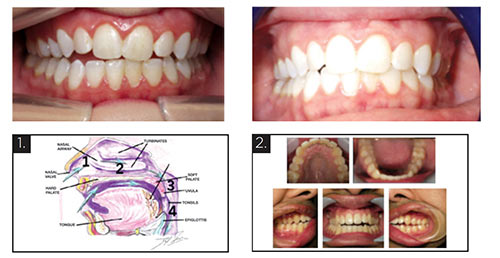
3D orthopedic development for pediatric Obstructive Sleep Apnea (OSA)
Orthodontic Practice US (Volume 7 Number 2) | March 31, 2016
This article seeks to evaluate the 3D volumetric changes that are necessary to treat pediatric Obstructive Sleep Apnea (OSA). Adult static therapies are not indicated for children. Children require dynamic therapies to encourage and correct skeletal development to improve sleep-breathing disorders. Formulas for arch width expansion are currently based on dental space and skeletal calculations and are not applicable nor are they validated in the treatment of pediatric OSA. Treating children with OSA requires a new formula of skeletal development for both maxilla and mandible based on correction of the immediate medical problem evaluated by overnight sleep testing called polysomnography (PSG) (attended) or home sleep testing (HST) (unattended).
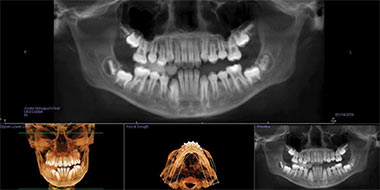
Optimal Dental Therapy for OSA
September 2015 | Dentalcetoday.com
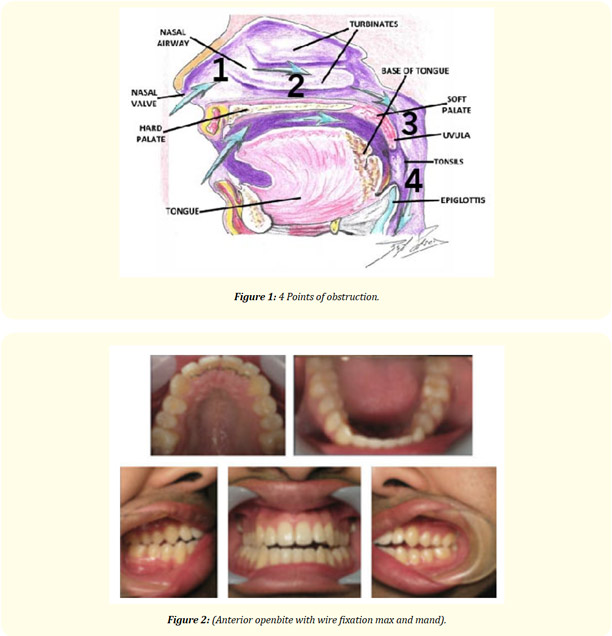
Optimal is a very different than acceptable, especially if you are the patient. This case study will highlight the need for a structural assessment of the 4 points of the airway prior to treatment utilizing CBCT (i-CAT). In additional, this case report will demonstrate how successful resolution of sever apnea with an oral appliance on a patient for whom continuous positive airway pressure (CPAP) had little effect on excessive fatigue until the nasal airway was addressed.
CBCT in the evaluation of airway — minimizing orthodontic relapse
Orthodontic Practice US | April 1, 2015
Dr. Steven Olmos Discusses the Four Points of Breathing Obstruction
For those of us who treat obstructive sleep apnea (OSA) or those who have tried but run into problems that make you want to throw up your hands, think about the four points of breathing obstruction. Each patient has a different set of obstructions, so decisions on how to choose between the hundreds of appliances to treat breathing disorders are based upon multiple points of obstruction. The best treatment may be combination therapy (hybrid): oral appliance therapy, nasal positive pressure, and nasal surgery. The optimal result is one in which the four points of obstruction are best managed. Triage of options is dependent on a good clinical exam of the tongue and its posture and cone beam computed tomography (CBCT).
Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015
Journal of Clinical Sleep Medicine | 2015
Introduction
Since the previous parameter and review paper publication on oral appliances (OAs) in 2006, the relevant scientific literature has grown considerably, particularly in relation to clinical outcomes. The purpose of this new guideline is to replace the previous and update recommendations for the use of OAs in the treatment of obstructive sleep apnea (OSA) and snoring.
Methods
The American Academy of Sleep Medicine (AASM) and American Academy of Dental Sleep Medicine (AADSM) commissioned a seven-member task force. A systematic review of the literature was performed and a modified Grading of Recommendations Assessment, Development, and Evaluation (GRADE) process was used to assess the quality of evidence. The task force developed recommendations and assigned strengths based on the quality of the evidence counterbalanced by an assessment of the relative benefit of the treatment versus the potential harms. The AASM and AADSM Board of Directors approved the final guideline recommendations.
Dentistry’s New Direction – “The Starting Point”
Oral Health | March 2014
by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO
I am so excited to be a dentist in the year 2014. I started out way back in 1977 as a freshman at the University of Southern California dental school wanting to help people by relieving their pain and preventing them from having it. As my practice evolved from giving relief from dental, bony and soft tissue infections, inflammation and injuries to the relief of Craniofacial Pain and Sleep Breathing Disorders, I am impressed. I am impressed and proud that we have a profession that is so expansive in its’ ability to help people that we can limit our services to addressing medical conditions as a Dentist.
Oral Health – Future of Dentistry (Part 3)
Oral Health | 2011
by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO
We need to evaluate our system of treatment. A patient presents with worn dentition or complaints of muscle soreness. The dentist produces a nightguard without further in vestigation. The result is that the treatment helps the symptom of muscle soreness, makes it worse or has no effect. The dentist is unclear what to do.
Use of a sibilant phoneme registration protocol to prevent upper airway collapse in patients with TMD
Gurdev Dave Singh & Steven Olmos
© Springer-Verlag 2007
Patients with temporomandibular dysfunction (TMD) require correction of mandibular position, but the ideal position for the mandible remains controversial. Miralles et al. [1] found the amount of freeway space (FS) required depended on the protocol used to measure it. For example, a significantly higher clinical FS value was found using a phonetic method than after swallowing or with the mandible in a relaxed postural position. A sibilant is the hissing or whistling sound heard in the formation of certain letters in speech, such as the letter “s.” A phoneme is the smallest unit of speech that defines one sound from another.


















